What to know about multiple sclerosis!

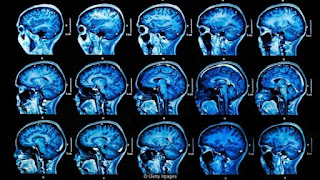
So, what is multiple sclerosis (MS) and how do you get it? MS is a chronic disorder where cells from the immune system attack the nerve cells of the central nervous system (CNS). There's a special substance called myelin, which covers the nerve cells and allows messages to pass from your brain to the body and vice versa. During a flare, the immune system attacks the myelin, the nerve covering becomes inflamed and communication between the brain and body is disrupted. The inflammation and nerve covering damage cause multiple areas of scarring (sclerosis) within the CNS, which is where the name multiple sclerosis originates. Unfortunately, the cause of MS is not yet known. Scientists believe that it could be caused by an unknown interaction of genetic predisposition and environmental factors. Which part of the body is affected and what are the symptoms? Since the central nervous system is made up of your brain, spinal cord, and specialized eye nerves, multiple sc...